For women who want to have children when the time is
right, egg freezing is a viable option and one that has become more popular in
recent years. As an abundance of fertility clinics pop up nationwide, it is
important to consider the safety implications of IVF, egg freezing, and
fertility clinics. Dive into the world of fertility clinics to understand how
eggs remain viable -- sometimes for years after harvesting -- and what risks the
environment holds.
How
Do Fertility Clinics Harvest and Store Eggs?
During the monthly menstrual cycle, women release a
viable egg. In the fertility harvesting process, IVF clinicians administer
hormones that increase egg production so they can harvest and store multiple
eggs in a one-time procedure.
Doctors first administer hormone injections to inflate
egg production prior to harvesting and storage. Three days after the final
injection, the eggs are ready for harvesting. At this point, female patients
then have eggs harvested from their ovaries using needles. Now the patient's
role is simply to leave the eggs at the IVF facility until she wishes to be
inseminated.
Traditionally, eggs were frozen for long-term storage,
then thawed out when patients wanted to use the eggs. This method worked, but
had a suboptimal success rate during IVF.
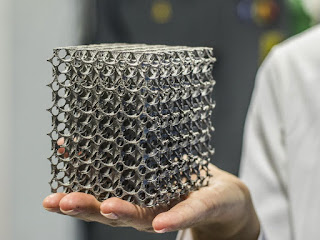
A new method, termed vitrification, increases the
success rate of egg freezing for in vitro fertilization. Vitrification uses a
flash freezing process to quickly freeze the eggs for long-term storage. After
the eggs have frozen, they are then stored inside tanks of liquid nitrogen
until they are needed. The new method reduces the formation of ice crystals,
which can damage the egg during the thawing out.
The main risk that doctors counsel patients on is the
chance that some or all of the eggs will perish in the process. Freezing of
eggs is still a relatively new procedure. However, there is a greater risk
involved. One that could affect female patients, their eggs, and fertility
clinic staff: The risk of liquid nitrogen exposure.
Nitrogen
Warnings in the Fertility Clinic Setting
Liquid nitrogen is perfectly safe as long as it
remains in storage tanks. If even a single tank were to develop a leak, and the
substance were to spill out into the fertility clinic, a lot more would be at
stake than the viability of stored eggs for in vitro fertilization.
Nitrogen has the potential to deplete oxygen from an
environment. At first, this may cause discomfort, dizziness, or confusion. As
the leak continues and displaces more oxygen from the room, staff can
asphyxiate. Since the gas cannot be seen or smelled, employees will not know
something is wrong until it is too late and lives are lost.
For the safety of clinic staff, an oxygen deficiency
monitor can be installed near the liquid nitrogen tank. This monitor takes
periodic readings of the oxygen levels in the room. When everything is working
properly and the oxygen is within the normal range, the monitor remains silent
yet vigilant. In a worst case scenario where a nitrogen leak does develop, the
O2 monitor will sound an alert once the oxygen in the room falls below
acceptable levels. The alarm gives staff enough notice to escape the premises
before being overcome by the lack of oxygen.
Like a carbon monoxide detector, an oxygen deficiency
monitor does not really do anything until something goes wrong but can save
lives in the event of an emergency. As with a carbon monoxide detector, it is
important to select and install a quality O2 monitor.
The latest generation of oxygen monitors from PureAire
come with a zirconium sensor, which requires no calibration or maintenance.
Staff can install the O2 monitor in the IVF facility and remain assured that it
will work for a period of 10 years with no maintenance of any kind.
For a reliable oxygen deficiency monitor, look to
PureAire, a company with over 15 years of experience in the field. Learn more
about PureAire's products at www.pureairemonitoring.com.